Rapid COVID tests! What you should know about accuracy
- Havilah Brodhead, RN, MSN, FNP

- Jan 14, 2021
- 6 min read
Updated: Jan 18, 2021


The skinny:
There are essentially two broad categories of testing:
1. Antigen test (frequently referred to as a rapid test). This test detects protein fragments specific to the Coronavirus. It can be done in a clinic, doctor’s office, or hospital. Turn around time for results is usually very quick and in some cases, results can be reported within 15 minutes.
2. PCR test. PCR testing is considered the “gold standard” in SARS-CoV-2 detection. This test actually detects RNA (or genetic material) that is specific to the virus and can detect the virus within days of infection, even those who have no symptoms. The test can be done in a clinic, hospital, or even in your car. Turnaround time is longer, generally in the 2-3 day range but results can be in as little as 24 hours. When demand is high, results can take a week or longer.
WHO SHOULD GET A RAPID TEST?
Rapid tests are considered most accurate in a patient who is having symptoms of COVID-19. While the rapid test can get you results very quickly, the results may not always be accurate.

Are rapid COVID-19 tests reliable?
To a certain degree, you’re sacrificing accuracy with speed. By their very nature, the antigen style tests aren’t as sensitive because they require a larger amount virus present to be positive. They can be helpful in rapidly screening symptomatic individuals early in the infection. They can also help to rapidly screen a large group of individuals during an outbreak in a resource-limited setting. Someone with a positive test by this style of test should be treated as infected with COVID-19, but a negative test is less reliable and may need to be confirmed by a more sensitive molecular assay.
WHAT DOES A FALSE NEGATIVE OR FALSE POSITIVE MEAN?
In those who don’t have symptoms, the false negative rate — meaning my test is negative but I actually have the disease — can be as high as 50%. This can have tremendous consequences as we try to contain the spread of COVID-19.
The false positive rate — meaning I test positive but I do not really have the disease — is quite low. So, if you test positive from a rapid test it is more likely you do have the disease.
BOTTOM LINE:
If you’re experiencing symptoms of COVID-19 and a rapid test result indicates you’re positive, you should take that as an indication you have the coronavirus. You should quarantine and contact your doctor.
However, if you have COVID-19 symptoms and a rapid test result is negative, you should still contact your doctor because you may need to receive a PCR test. Don’t be victim of a false sense of security with a false negative result from a rapid COVID-19 test.
WHAT IF I HAVE A NEGATIVE RAPID TEST BUT STILL HAVE SYMPTOMS?
Current recommendation is to have a confirmation test performed (the PCR test) if you still have symptoms and have had a negative rapid test. This is especially true if you’ve had a high-risk exposure. A high risk exposure is considered more than 15 minutes of contact with a COVID-positive individual in a 24-hour period and you have been within 6 feet of this individual.
Keep in mind there are still high false negative rates with the PCR test. Typically I order a respiratory PCR panel which looks for other viruses that could be causing a patient's symptoms if their covid test is negative.
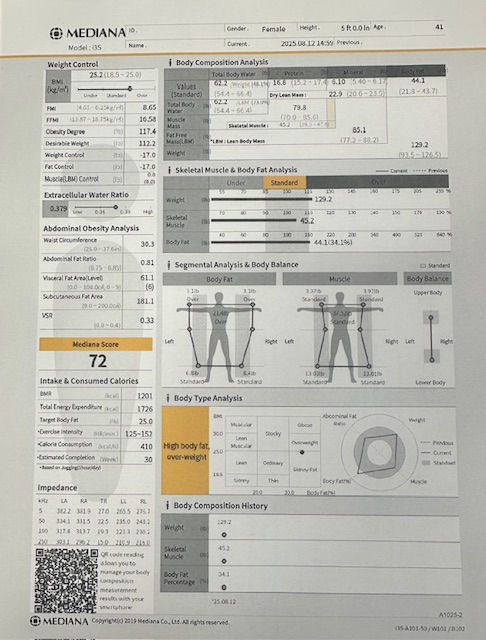
This is a photo of a respiratory PCR panel I recently ordered on a patient's who COVID test came back negative, to look for other viruses:

And for those wanting more detail---keep reading!
Molecular tests (also called PCR tests, viral RNA tests, nucleic acid tests)
What about accuracy? The rate of false negatives — a test that says you don’t have the virus when you actually do have the virus — varies depending on how long infection has been present: in one study, the false-negative rate was 20% when testing was performed five days after symptoms began, but much higher (up to 100%) earlier in infection.
The false positive rate — that is, how often the test says you have the virus when you actually do not — should be close to zero. Most false-positive results are thought to be due to lab contamination or other problems with how the lab has performed the test, not limitations of the test itself.
A molecular test using a nasal swab is usually the best option, because it will have fewer false negative results than other diagnostic tests or samples from throat swabs or saliva. People who are in the hospital, though, may have other types of samples taken.
Antigen tests
How is it done? A nasal or throat swab.
Where can you get these tests? At a hospital, a doctor’s office or at home (the FDA has authorized a home antigen test that requires no prescription).
What does the test look for? This test identifies protein fragments (antigens) from the virus.
How long does it take to get results? The technology involved is similar to a pregnancy test or a rapid strep test, with results available in minutes.
What about accuracy? False negative results tend to occur more often with antigen tests than with molecular tests. This is why antigen tests are not favored by the FDA as a single test for active infection. Because antigen testing is quicker, less expensive, and requires less complex technology to perform than molecular testing, some experts recommend repeated antigen testing as a reasonable strategy. As with the molecular test, the false positive rate of antigen testing should be close to zero.
“You don’t need complex and expensive test kits to detect the antigens,” Tran said. “That makes them cheaper and faster. The problem is, there is a little lag time between when someone gets infected and when the antigens show up.”
That means, if a person is not near peak infection – but is still contagious – the tests may come back negative. Depending on the quality of the antigen test and the test takers, false negatives results can be very high.
“Here’s a good way to look at this,” Tran said. “The coronavirus replicates itself by putting its genetic material inside our cells. If you’re testing that person at the stage when the virus is still replicating inside the cells, it has not produced sufficient protein or shed in large enough amounts to be detected yet by antigen testing.”
The Centers for Disease Control and Prevention (CDC) has advised people who show COVID-19 symptoms but test negative with a rapid antigen test (or who have had a recent close contact exposure) to get a PCR test to confirm the results.
Tests for past infection
An antibody test can show if you have previously been infected with the COVID-19 virus.
Antibody tests (also called serologic testing)
How is it done? A sample of blood is taken.
Where can you get these tests? At a doctor’s office, blood testing lab, or hospital.
What does the test look for? These blood tests identify antibodies that the body’s immune system has produced in response to the infection. While a serologic test cannot tell you if you have an infection now, it can accurately identify past infection.
How long does it take to get results? Results are usually available within a few days.
What about accuracy? Having an antibody test too early can lead to false negative results. That’s because it takes a week or two after infection for your immune system to produce antibodies. The reported rate of false negatives is 20%. However, the range of false negatives is from 0% to 30%, depending on the study and when in the course of infection the test is performed.
Research suggests antibody levels may wane over just a few months. And while a positive antibody test proves you’ve been exposed to the virus, it’s not yet known whether such results indicate a lack of contagiousness or long-lasting, protective immunity.
The true accuracy of tests for COVID-19 is uncertain
Unfortunately, it’s not clear exactly how accurate any of these tests are. There are several reasons for this:
· We don’t have precise measures of accuracy for these tests — just some commonly quoted figures for false negatives or false positives, such as those reported above. False negative tests provide false reassurance, and could lead to delayed treatment and relaxed restrictions despite being contagious. False positives, which are much less likely, can cause unwarranted anxiety and require people to quarantine unnecessarily.
· How carefully a specimen is collected and stored may affect accuracy.
· Because these tests are available by EUA, the usual rigorous testing and vetting has not yet happened, and accuracy results have not been widely published.
· A large and growing number of laboratories and companies offer these tests, so accuracy may vary.
· All of these tests are new because the virus is new. Without a long track record, assessments of accuracy can only be approximate.
· We don’t have a definitive “gold standard” test with which to compare them.
How much does testing cost?
Cost varies widely, from under $10 to hundreds of dollars, depending on whether your health insurance will cover the test, or if you’ll be paying out of pocket. It also depends on which test you get and where it’s done. We STRONGLY advise you find out with your insurance company what they will cover before getting these tests done so you have no hidden suprises.
We'd like to thank the following resources for the compilation of this blog:
https://www.memorialhealthcare.org/whats-the-difference-between-covid-19-rapid-and-prc-tests/





Comments